Type 2 inflammatory responses involve both innate and adaptive immune systems and are triggered by exposure to infectious pathogens and environmental antigens, as for example helminths, allergens, and venoms. These responses are characterized by activation of T helper 2 cells and subsequent release of type 2 cytokines, such as interleukin-4 (IL-4), IL-5, IL-9, and IL-13, resulting in production of immunoglobulin E (IgE) and activation of different types of effector cells—basophils, mast cells, and eosinophils. Typically, these responses promote increased mucus production and muscle contractions which, together, help to expel the parasite or allergen from the body.
Group 2 innate lymphoid cells (or ILC2s for short) are a potent source of type 2 cytokines and therefore are involved in type 2 inflammatory responses. These cells are present in human lung tissue, peripheral blood, gastrointestinal tract, skin, and sinonasal tissue, and likely contribute to chronic rhinosinusitis, asthma, atopic dermatitis, and gastrointestinal allergic disease.
Results from a study published last year in the scientific journal Science (2-adrenergic receptor–mediated negative regulation of group 2 innate lymphoid cell responses) show that ILC2s are involved in a crosstalk between the nervous and the immune system, thus playing an important role in regulating acute and chronic inflammation. But what are the mechanisms at the basis of these regulatory processes?
Researchers used mice to discover that ILC2s express the β2-adrenergic receptor (β2AR) and are located in the intestine in close proximity to adrenergic neurons. Adrenergic neurons release either the neurotransmitter adrenaline (epinephrine), or noradrenaline, or dopamine, which interact with β2ARs—β2ARs give nerve cells the ability to interact with each other and influence the immune response.
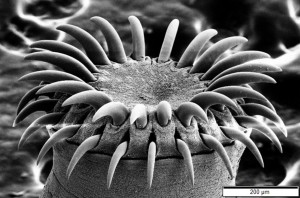
The researchers then infected mice that lack β2ARs with the gastrointestinal helminth Nippostrongylus brasiliensis, which was already known to induce potent ILC2 responses that play an important role in the expulsion of the parasite through production of IL-5 and IL-13. These mice had exaggerated ILC2 responses to the helminth infection in intestinal and lung tissues resulting in faster expulsion of the parasites. By contrast, when they treated normal mice with drugs that stimulate β2AR, the immune response was blunted and the helminth infections worsened. In addition, the researchers found that the β2AR pathway negatively regulates the ILC2 responses through inhibition of cell proliferation and effector functions. Collectively, these data provide the first evidence of a neuronal-derived regulatory circuit that limits ILC2-dependent type 2 inflammation. All together, the study results highlight a previously unrecognized regulatory circuit that operates between the adrenergic nervous system and the innate immune system to control type 2 inflammation at multiple mucosal sites.
The most commonly used drugs to treat asthma also stimulate β2AR, which may explain why they are so effective at controlling allergy symptoms. David Artis, senior author of the study, said in a press release: “We must have given tens of millions of doses of these drugs to shut down the acute symptoms of asthma. Nobody could agree on how these drugs work, but it may be that they are working in part through targeting the innate immune system. If we understand more mechanistically how this class of drugs works, it might give us new avenues to develop additional therapies built around the biology.”
In their published paper, the researchers conclude that the mammalian nervous system appears to have evolved dual mechanisms to rapidly activate or repress group 2 innate lymphoid cells to protect the host against diverse inflammatory stimuli.

After reading the whole article I have knowledge that inflammatory responses are concerned in the innate and adaptive immune system are activated by exposure to infectious pathogens and ecological antigens. This response is considered by activation of T helper 2 cells and subsequent release of type 2 cytokines which result to production of immunoglobulin E (IgE) and effector cells, for example, eosinophils which increase mucus production and muscle contractions to expel the allergens. Moreover, the researchers found that ILC2s are involved in the crosstalk between the nervous and the immune system; hence help in regulating chronic and acute inflammation. In addition, the adrenergic receptor pathway negatively regulates the ILC2 responses via inhibition of cell proliferation and functions of effectors. Most asthma drugs stimulate the adrenergic receptor which controls allergy symptoms. In my opinion mammalian nervous system appears to have evolved dual mechanisms to activate group 2 innate lymphoid cells rapidly to protect the host against diverse inflammatory stimuli.
https://www.ncbi.nlm.nih.gov/pubmed/30018263
This article proved interesting in highlighting how aspects of the immune system can at times work for our benefit, while at other times proving to be a detriment to recovery from illness. The article makes mention of the helminth parasites’ ability to trigger ILC2 responses and result in inflammation; in addition to this, the Notch pathway plays a pivotal role in this immune response. In an experiment by researchers at Cornell University using mice, it was shown that upregulation of the Notch pathway in basophils tends to result in them localization in the area of infection and the mass release of cytokines and ILC2. When the Notch pathway was down-regulated or removed entirely, basophilic activity declined even in the presence of cytokine stimulation, resulting in lowered inflammatory response and impaired infection recovery. It is likely that the B2AR downregulation and the Notch pathway upregulation work in tandem to speed up and exaggerate the inflammatory response and clear parasitic infections quicker.
https://www.ncbi.nlm.nih.gov/pubmed/30975892
In reading the post, I started thinking back to my neuroscience courses, where one of the fundamental concepts learned was that a neurotransmitter has distinct physiological effects depending on the receptor it binds. For example, acetylcholine stimulates muscle contraction when it binds to nicotinic acetylcholine receptors in skeletal muscle. Conversely, acetylcholine inhibits muscle contraction upon binding to muscarinic acetylcholine receptors in cardiac muscle. This duality of neurotransmitters reminds me of the interconnectedness of biological systems and how our physiological processes comprise an intricate overlapping network. Primary and secondary lymphoid organs are innervated by the sympathetic and parasympathetic nervous systems of the autonomic nervous system, but a lot of these mechanisms are not entirely understood. This is why the article in the post is relevant because the authors of the study found more information on the circuit for ILC2s and adrenergic neurons regarding the Beta-2 adrenergic receptors.
Accordingly, I sought to search for other understood mechanisms in which Beta-2 adrenergic receptors interact with components of the immune system. This study found a mechanism by which signaling from β2-ARcan inhibit CD8+ T cell activation is via suppression of the metabolic events. This finding is indicative of a novel mechanism for how adrenergic stress can suppress the effector activity of the immune cell. These findings of the studies mentioned are important because they could help yield novel therapeutic agents for immune disorders.
https://www.ncbi.nlm.nih.gov/pubmed/30229289