In March 2013, a new flu virus — the H7N9 — was identified in China. By early May, before retreating and disappearing, it had infected 131 people and killed 26 of them. However, a few months ago (January 17, 2104), the New York Times reported that “China is disclosing a steadily growing number of cases of H7N9 bird flu, including four more cases announced on Friday, reviving concerns among health experts that the disease may be spreading and could pose a further threat as the world’s largest annual human migration begins ahead of Chinese New Year.” On May 17, China reported two new human H7N9 cases.
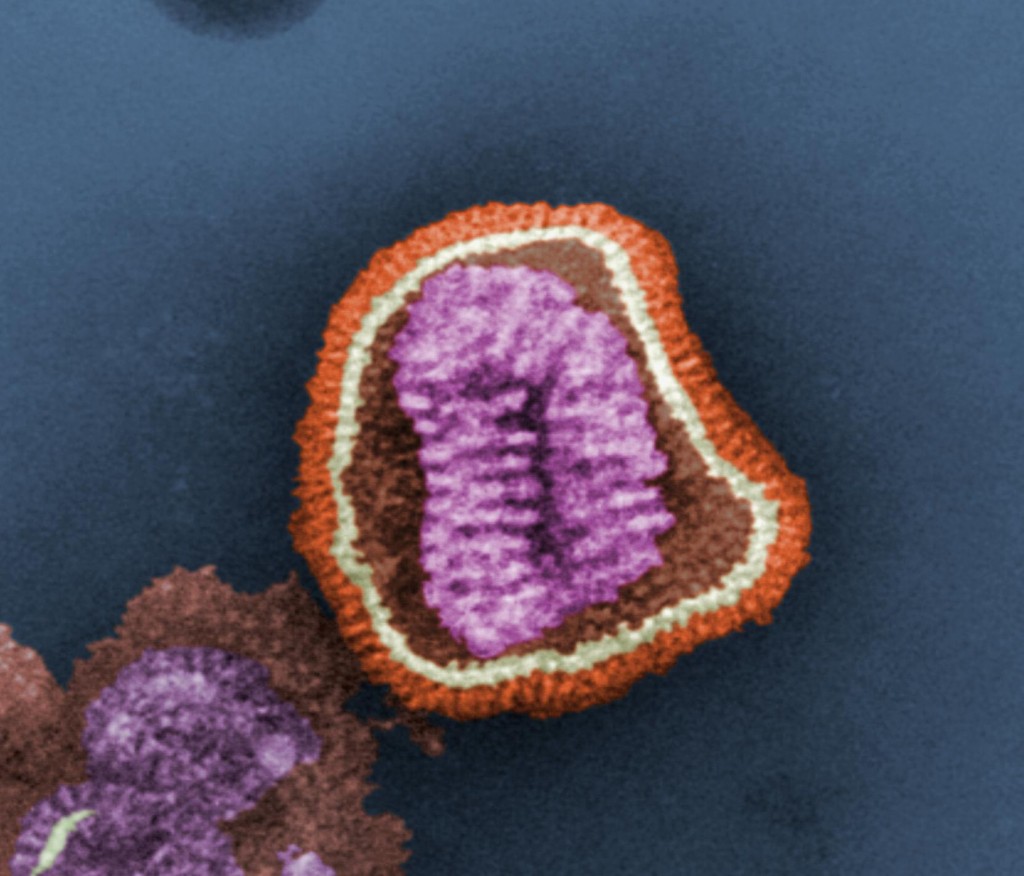
The H7N9 virus is a “reassortant” — it includes combined elements from three distinct viruses. People acquire the virus mostly from exposure to infected poultry. As of today (May 22, 2014), the World Health Organization states that there is no evidence of sustained person-to-person spread of H7N9.
According to the Centers for Disease Control and Prevention (CDC), “It’s likely that sporadic cases of H7N9 associated with poultry exposure will continue to occur in China. Cases associated with poultry exposure also may be detected in neighboring countries. It’s also possible that H7N9 may be detected in the United States at some point, possibly in a traveler returning from an affected area. Most concerning about this situation is the pandemic potential of this virus.”
During pandemics, which are caused by the worldwide spread of infectious microbes, different human populations respond differently to the infection, most likely because of specific differences in factors related to their immune system.
Is this also true for the H7N9 virus? Should we expect differences in the susceptibility of different populations to infection?
An international team of investigators from institutions in Australia, Singapore, the U.S. and the U.K. report, in an article recently published by the journal Proceedings of the National Academy of Sciences USA (January 21, 2014), that different human populations may indeed vary in their susceptibility to H7N9 infection. The article is titled “Preexisting CD8+ T-cell immunity to the novel H7N9 influenza A virus varies across ethnicities” and presents results related to several ethnic groups, including Caucasoid, North American natives, Oriental, African, Amerindian, Alaskan Yupik and Australian Aboriginals.
Because H7N9 is a “new” virus, the immune system does not have memory of it and it is not ready to quickly produce neutralizing antibodies — which protect from infection or severe disease — when it encounters the virus. In absence of neutralizing antibodies, the human immune system relies mostly on a type of killer cells — called cytotoxic T lymphocytes — for protection against the virus. These lymphocytes kill cells infected with the virus along with the virus growing in them.
However, cytotoxic T lymphocytes can kill infected cells only if viral peptides — short segments of the viral proteins — are bound, in the infected cells, to molecules called HLA. Many of the peptides from the H7N9 flu virus are very similar (“conserved”) to peptides from other flu viruses with which human populations have already been in contact, and cytotoxic T lymphocytes that “remember” these peptides are ready to kill cells infected by H7N9.
There is a caveat, though. HLA molecules are present in the human population in a very large number of variants, and not all variants are able to bind the same peptides. Consequently, some human populations may not have HLA molecules that bind H7N9 peptides and, therefore, may not use quick-acting cytotoxic T lymphocytes to eliminate the virus.
Results from the study show that Alaskan and Australian Indigenous people do not have HLA variants able to bind the “conserved” H7N9 peptides and, therefore, may be particularly vulnerable to H7N9 infection.

Luckily there has not been any transmission human to human and the only spread to humans is associated with poultry. However, the influenza virus is a segmented RNA virus. Both are key features that allow this virus to change through either recombination or mutation. Due to this we need to quickly develop a vaccine to get a better handle on this virus before it changes and is able to spread from human to human, especially because there are people with immune systems that are unable to recognize the virus. The vaccine wouldn’t be useful for them in the sense of boosting their immune response, however with a vaccine would herd immunity then play a role in helping lower the chances of them getting the virus?
I doubt that vaccinating certain members will grant the population herd immunity since the virus is only transmitted via poultry to humans. If the unvaccinated person were to eat infected poultry, they would still contract the virus regardless of if those around him are vaccinated. The only way for a vaccine to be effective, since the flu is asymptomatic in birds, is likely to vaccinate all of the poultry entering the country. If the poultry is vaccinated, they hopefully won’t become infected and pass it onto those who do not have the necessary HLA molecules to fight it off.
I find it interesting that certain ethnic groups have more of a defense mechanism against this new Influenza virus, as oppose to other ethnicities. Due to the lack of recognition they are more susceptible to viruses because they have no memory cells of the H7N9 present. I believe more initiative needs to be taken by the government of these indigenous countries by having vaccines put into place, so that more people are protected from these infections. Likewise, people are affected with this virus because of infected poultry so more stricter food safety precautions need to be put into place so that these kinds of threats to ones immune system are controlled.
As you mentioned in the posting, H7N9 virus is a combination of three known viruses. This made me think that the three viruses related to H7N9 are also found in China. Just like humans, viruses as well as the molecules in our body mutate and evolve throughout the years. With evolution, natural selection plays an important role. If a feature is not needed, it slowly goes away. Perhaps the people living in Alaska and Australia were never exposed to the three viruses that make up H7N9 and therefore do not have the HLA variants necessary to bind to the peptides. This made me curious; it is possible for HLA molecules to evolve geographically with the human population?
I found a blog that discussed this similar idea. http://lifescienceexplore.wordpress.com/2014/01/17/some-ethnic-groups-more-susceptible-to-h7n9-bird-flu/ Since Alaska and Australia are geographically remote; their exposures to viruses have been fewer than most countries. If the presence of the other three viruses were prevelant in Alaska and Australia, the HLA molecules in the people living there could have evolved helping their immune system.
Lesser developed areas in China and Asia often have people living in close quarters with animals, especially in the market areas where people sell chicken, pig, and other wild animal products, and small home farms where people keep small amounts of livestock. Of course, these products are not handled and stored properly, at least by FDA and USDA standards. Having live and freshly killed chickens and pigs in close proximity to humans is the perfect combination of conditions necessary for a major influenza shift event. In a recent 2014 study tracing H10N8 through Nanchang, China, researchers stated that in live-poultry markets, “the sale of freshly slaughtered poultry, live poultry transportation, and mixed trading of different domestic animals provide environments conducive to genome segment reassortment, gene mutation, and interspecies transmission of AIVs.” Pigs, chickens, and humans are the three species of animals in which the large majority of interspecies transmission of influenza strains occurs. This occurs when a single animal is infected with two unique strains of influenza, for example H10N2 and H5N7. Because influenza is a segmented virus, it has the ability to undergo genetic reassortment (ie. antigenic shift), to create a novel strain of virus. In this example, H10N7 may result. Markets and farms in close proximity to humans in these lesser-developed countries are where epidemics and pandemics begin, as people will not have antibodies to these novel viral strains. Fortunately, many novel influenza strains cannot infect additional humans after jumping the species barrier from pig to human or bird to human – the virus will need to undergo mutation/drift events in order to obtain the right characteristics for this to occur.