The Human Immunodeficiency Virus (HIV) continues to be a major global public health issue, having claimed more than 39 million lives so far. According to the most recent fact sheet on HIV/AIDS (Fact sheet N°360) published by the World Health Organization (WHO), about 1.5 million people died from HIV-related causes in 2013, globally. There were approximately 35.0 million people living with HIV at the end of 2013, with 2.1 million people becoming newly infected with HIV in 2013. There is no cure for HIV infection. However, effective treatment with antiretroviral drugs can control the virus so that people with HIV can enjoy healthy and productive lives. In 2013, 12.9 million people living with HIV were receiving antiretroviral therapy globally.
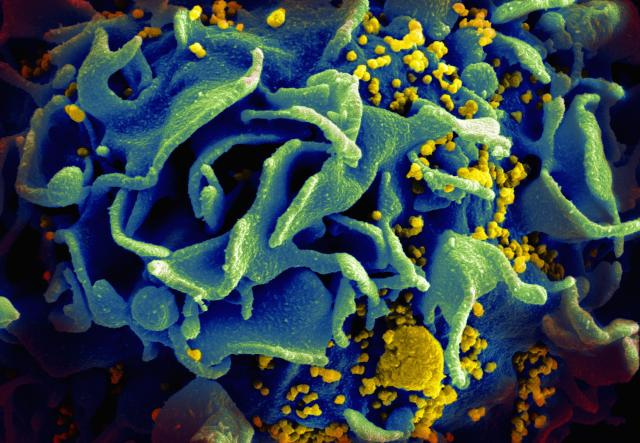
HIV is a lot like other viruses, including those that cause the flu. However, while the immune system can clear most viruses out of the body, this isn’t the case with HIV — the human immune system can’t seem to get rid of it. Indeed, HIV can hide for long periods of time. It attacks a key component of the immune system – the CD4 T cells. These cells are necessary to fight infections and diseases, but HIV invades them, uses them to make more copies of itself, and then destroys them. In addition, it can hide in them in its so-called “latent” form.
When first diagnosed with HIV infection, patients start a form of therapy called highly active antiretroviral therapy (HAART). But, what is HAART, exactly? HAART is a customized combination of different classes of medications that a physician prescribes based on such factors as the patient’s viral load (how much virus is in the blood), the particular strain of the virus, the CD4 T cell count, and other considerations (for example, disease symptoms). While HAART can control HIV almost completely, the virus can still replicate at low levels and accumulate in the latent form in what are called “reservoirs.” The problem is that HAART does not reach these reservoirs, which are located throughout the body, including the brain, bone marrow and genital tract. Thus, the virus contained in the reservoirs can lead to disease progression and cause complications and deaths due to non-AIDS related diseases.
Now, results from a new study show that a vaccine consisting of an HIV protein called “Tat” can induce an immune response that prevents disease progression in patients undergoing HAART. Tat is produced early on in HIV infection, and plays a key role in viral replication and progression of the disease by weakening the immune system.
The researchers conducted a Phase II clinical trial by injecting 168 HIV-infected patients with either 7.5 micrograms or 30 micrograms of the Tat protein. At the beginning of the trial, patients were not producing antibodies directed against the Tat protein — however, it was anticipated that they would start producing anti-Tat antibodies after receiving the vaccine. Patients received the vaccine once a month over the course of either three or five months while continuing HAART treatment, and were followed for three years.
Results from the study show that the vaccine induced production of anti-Tat antibodies, and a significant increase in the number of CD4 T cells. The best response was seen amongst those who received 30 micrograms of Tat over the course of three months. In addition, the Tat vaccine significantly reduced the proviral DNA load, which is the latent form of the virus that accumulates in reservoirs. It is noteworthy that CD4 T cell numbers continued to increase — while levels of proviral HIV DNA continued to decrease — three years after the first immunization.
The researchers are currently awaiting to confirm their promising findings with results from a phase II double-blinded trial that has taken place in South Africa.

HIV is one of the most deadly viruses circulating in the world’s population today. Until recently, most of the therapeutic research had been based on developing a vaccine that induces broadly neutralizing antibodies against this virus but this approach has not been successful because HIV mutates very quickly and antibodies are specific. The Tat protein is an early gene regulatory gene that is necessary for viral replication. Targetting this protein is a promising approach because it is well preserved and is necessary for the virus to replicate itself. Even if the virus is able to infect a cell, if it cannot replicate then it cannot integrate it’s genome into the host’s and the disease cannot progress to AIDS. As mentioned in the article above, the Tat vaccine has also been shown to promote the restoration of CD4 and CD8 T-cells.
What about using the Tat vaccine to prevent healthy people from being infected with HIV? Over the last 30 years, only 4 vaccines have been tested in efficacy trials. Previous vaccine studies have used anti-Env antibodies which attach to the viral envelope proteins in order to block entry of the virus into target cells. However in the presences of anti-Env antibodies, extracellular Tat form a Tat/Env complex redirecting the virus to RDG-binding integrins on the targets cell which allows the virus to enter the cell. When monkeys were vaccinated with anti-Env and anti-Tat (HIV-1 tat promotes integrin-mediated HIV transmission to dendritic cells by binding Env spikes and competes neutralization by anti-HIV antibodies), HIV entry was blocked and no infection was detected even when the monkeys were injected with a highly virulent form of the virus. Anti-Tat has been tested on humans for safety but has not been tested for efficacy as yet.
I agree that running more tests to see if the Anti-TAT vaccine is successful is an important next step. Since TAT regulates the viral transcription’s efficiency, blocking it seems like a good way to stop HIV from initiating a positive feedback cycle. Once inside the body, it can affect non-HIV cells by causing apoptosis. This can eventually lead to AIDS if not maintained. Testing on Chinese individuals that are infected with HIV-1 has been performed. It is still unclear how the TAT antibody works, but there is some evidence that supports the stopping of transcription.
I decided to look more into the Tat vaccine and I came across the Italian National AIDs center. I noticed that there were a few different generations of the Tat vaccine. The first generation, which was only the Tat, required to be stored at -80°C. The first generation was found to be safe and had no adverse side effects, and it resulted in an immune response in the vaccinated patients.
One obvious problem I came thought of was the logistics of storing it at such a low temperature, specially in third world countries that do not always posses the means possible to store it at that temperature. To solve this issue, the second generation vaccine included micro-particles. In pre-clinical studies they found that the second generation could room temperatures. However, the micro-particles could damage the antigen. To solve the problem, scientists at the University of Piemonte Orientale developed micro-particles that are able to reversibly bind macromolecules to their surface.
I think that this step of making different generations of TAT vaccine is a smart idea since it is known that AID tend to spread rapidly in Africa and Asia and it has threatened other people’s lives and safety worldwide more than other diseases. Therefore, the local and global cooperation would strength the health services provided and make the TAT vaccine accessible and be effective in generating immune response that limits the progression of the disease.
According to the research information available about transactivator (Tat) protein’s function should create an understanding that it may be futile for a Tat vaccine to prevent health people from being infected with the deadly Human Immunodeficiency Virus (HIV) at this point in time. According to a review article The HIV-1 Tat Transactivator Protein: a Therapeutic Target?, state: “Central to HIV infection is the transactivator protein Tat, that plays a critical role in the nucleus during the HIV infectious cycle, by binding the transactivation-responsive region (TAR) and thereby enhancing transcriptional elongation.” However, I do not negate the fact that it is impossible to prevent healthy people from being infected with HIV, as future research on this Tat protein may show promise later on. Yet, it is a long road to travel while the death toll increases rampantly. Further research by Alex J. Fulcher and David A. Jansunderstanding shows that “blocking Tat nuclear import is likely to prevent HIV infection…” This is important for accessing the therapeutic capabilities of Tat.
The anti-seizure medication Valproic has been shown to to activate cells that contain the latent virus. HIV medication that are prescribed today are only effective on cells that are actively producing the virus. I would be interested to see if a new form of HAART, that started with the TAT vaccine and was coupled with Valproic, would be effective in eliminating the virus from an infected person permanently. Valproic has many serious side effects however and much more research needs to be done before this drug could be considered in a treatment plan for HIV patients.
The results from this study are very assuring that HIV can be conquered and that individuals with HIV can have a normal life expectancy. According to The Bulletin on AIDS Research, most of developed HIV vaccines involve the incorporation of enveloped proteins in which the course of designing it is difficult since the HIV enveloped proteins has the tendency to change their structural forms. Therefore, Tat vaccines can provide an alternative method to induce cellular immunity more effectively since Tat vaccine causes the increase in CD4 T cells, which activate other immune cells to generate a response against the infection instead of failed attempts of other HIV vaccines to cause a complete immune protection
Is a “new vaccine” really the answer to successfully combating the HIV/AIDS epidemic and for whom would the “improve efficacy” of antiviral therapy be available? The answer to these questions may come upon an approach of a new vaccine for HIV/AIDS. Even though there are newer treatments that dramatically improve both the quality of life and life expectancy of people with HIV, they aren’t available to everyone needing them. It may very well be that research science is fighting a battle that nature has deemed implausible of winning.
May 20 marks HIV/AIDS Vaccine Awareness day and the United Nations Program on HIV/AIDS or UNAIDS is calling for sustained funding in efforts of developing a new vaccine. According to Executive Director Michel Sidibe, “A vaccine would be a major step towards ending the AIDS epidemic.” However news article, UN Agency Calls for Renewed Global Commitment to Develop Effective HIV Vaccine mentions that in “2013 HIV vaccine research and development dipped to its lowest decline since 2008.” Moreover, the success of transforming the concepts already known about HIV/AIDS into an effective vaccine requires sustained funding be maintained.
Then, there is another challenge posed to how beneficial a new vaccine for HIV/AIDS will be to developing country’s population such as the tropics, sub-Saharan African and India among others, since there are complications to acquiring affordable drugs. According to a magazine article by Elizabeth Hilton, A Bitter Pill for the World’s Poor mentions such complications to be trade restriction, policy, the interest of the pharmaceutical industry, and intellectual property rights. Hilton further mentions that the pharmaceutical companies judge that they would not get sufficient returns on research investment as the hold an obligation to its shareholders.
It does not seem promising that a new HIV/AIDS help in its eradication since many people in developing nations are poverty stricken, the vaccine may be unaffordable, and there may be no market. There lies great promise in finding a vaccine with improved efficacy, as the United States has come a long way judging by the significant decline in HIV infection in infants due to prophylactic therapy and antiviral (ARV) drugs. It is with great hope that on the dawn of finding a HIV/AIDS vaccine with enhanced efficacy, it is made accessible and affordable.
HIV is one of the most deadly viruses and is very difficult to target due it its retroviral aspects and its latent stage. The use of HAART and targeting the viral co-receptor CCR5 on CD4+ T cells for blockage and gene editing has been constantly and consistently researched by scientists, and these types of therapies may provide resistance to those that are not infected with HIV. The issue is for those whose cells are currently infected with the virus, especially if it is latent. Serum transfer can only be done so many times before it causes sickness, and the massive amount of T cells that have been destroyed is overwhelming, causing serious immune deficiency. In addition, even if all the cells that have current active infection are destroyed, the possibility of a latent virus becoming active and taking over the body once more is great.
Hearing about this new vaccine is exciting because by altering the disease progression, preventing replication, and increasing the immune response, an infected patient may actually have a fighting chance.
HIV/AIDS patients take many different medications. An important next step is answering the question what can not be ingested with this new vaccine? Although it seemingly works well in conjunction with the HAART therapy, can it be used with other drugs such as protease inhibitors? Does the vaccine benefit the body more than it hurts it? Many HIV drugs have dreadful side effects. Hopefully, this vaccine is a better answer.
Seeing that our own immune system can effectively find and kill cancerous calls makes me wonder. If scientists found a way to rapidly and effectively proliferate our own CD8+ T cells in the early stages of cancer, they could eradicate most of the cancer. Then, chemotherapy can be included in treatment. I feel like more would survive if we could boost our own killers then call for backup when needed. Also chemotherapy has many negative side effects such as hair loss and nausea. An alternative route to treating cancer is needed.
Wrong article. Apologies.
This is a great step in the right direction with HIV medication research. Sorry for just going off memory here, but I want to talk more in detail about HAART. Just a quick summary of it is that HAART is a cocktail of many different medications that are adjusted depending on each patient. Because it cannot affect the reservoirs of HIV in patients it has to be taken daily by the patient to keep the virus at bay. But the problem is HIV tends to become resistant to the cocktail blends fairly rapidly, so they will up the dosages or change the blend. This can work for a time but the same issues can keep occurring. Also when the dosages are increased the side effects tend to become more severe to the point of people not wanting to take the medications anymore.By the looks of this paper the rate of HAART not working is not as bad as what my microbiology professor explained to us, but still does not look to be the best looking prognosis.
The Tat vaccine and heart treatment working in tandem makes for a dynamic combination. From what I’ve gleaned about HAART from Wikipedia is that each part of the drug cocktail is designed to inhibit a separate part of the viral life cycle. Such as attachment, reverse transcriptase inhibitors, and integrase inhibitors to name a couple. However this is less effective in reality, because recruiting these drug chemicals to the site of the retroviral reservoirs is a shot in the dark. What is novel about this new Tat treatment, is that it’s a vaccine. It is a vaccine that results in production of Tat binding antibodies. Since antibodies are part of your humoral immunity, their circulation in the blood ensures they are more likely to encounter zones of disease reservoirs where the latent viral protein will be abundant. When the immune system has all of its parts in working order, even compared to laboratory designed chemicals, it is our best means of defense against foreign invading pathogens. These two techniques together can halt disease progression. This is good news, and some of the most hopeful research in HIV to date. Yet still this not an avenue to finding a cure. This is a means of managing symptoms of HIV. If I had the resources I would inoculate non-infected individuals with a Tat vaccine and see how that effects disease progression after HIV infection. Would the potential lag these antibodies cause the viral setup be enough to prevent a rooted infection and possibly remove the pathogen once again entirely? As for the model organism, This could possibly be done on mice or monkeys. Human Immunodeficiency Virus is specific to humans, but perhaps homologous analogues could be used to deliver some poignant information on the question.