During the past few years, the global fight against tuberculosis (TB) has made noticeable progress: according to the World Health Organization, between 2000 and 2013, over 37 million lives have been saved through effective diagnosis and treatment. However, as detailed in the Stop TB strategy, much more needs to be done. One of the targets of this strategy is to eliminate tuberculosis as a public health problem by 2050.
Despite the considerable progress in saving lives, the death toll is still enormous. In 2013, an estimated 9.0 million people developed tuberculosis and 1.5 million died from it. The disease frequently has devastating economic consequences for affected families, reducing their annual income by an average of 50%, and aggravating existing inequalities. A few days ago, Margaret Chan, WHO Director-General, said in a press release: “This is a matter of social justice, fundamental to our goal of universal health coverage. Each and every man, woman or child with TB should have equal, unhindered access to the innovative tools and services they need for rapid diagnosis, treatment and care.”
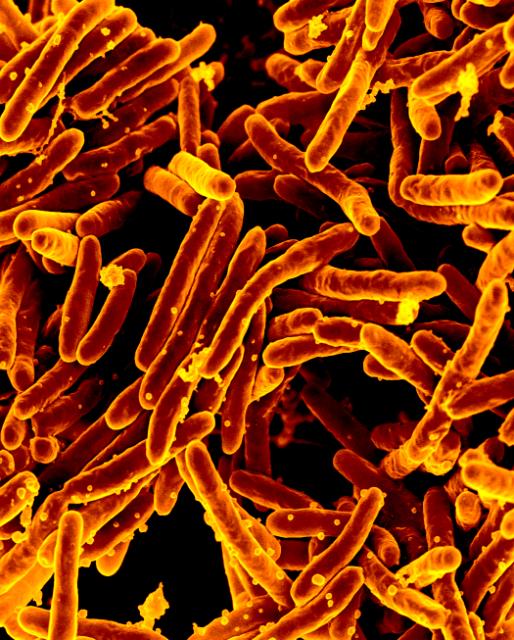
However, the most effective way to stop the global tuberculosis epidemic is to prevent the spread of Mycobacterium tuberculosis — the infectious microorganism that causes the disease — through the use of effective vaccines. The only tuberculosis vaccine currently available, Bacille Calmette-Guérin, or BCG for short, has only limited efficacy. It is used in countries where the incidence and prevalence of TB is high. BCG has been available for almost a century, and is the most widely used vaccine in the world — unfortunately, its use has not eliminated tuberculosis. BCG can protect children from the most severe forms of tuberculosis, but it has little to no efficacy in preventing pulmonary tuberculosis in adults, the most common and most infectious form of the disease. Indeed, modeling studies published in 2009 show that tuberculosis cannot be eliminated without new vaccines and mass vaccination campaigns. Prevention through vaccination is expected to be the most cost-effective tool in the control and eradication of tuberculosis.
During the past ten years, more than 15 tuberculosis vaccine candidates have been evaluated in more than 50 human trials, requiring global investments of more than 600 million US dollars. Over the next decade, the results of these trials will allow to assess the efficacy of the vaccine candidates.
According to Aeras, there are still scientific challenges facing the development of tuberculosis vaccines:
- A lack of understanding of how vaccines work or the protective immunity against TB in different age groups and populations
- No correlate or surrogate endpoint of protective immunity, meaning new TB vaccines cannot easily be evaluated in experimental animal models or in early clinical trials
- The current need to evaluate vaccine efficacy in long, protracted and costly clinical trials
- Large gaps in our understanding of TB, the way our natural immune system responds to TB infection, and antigen identification and selection
BCG is currently given to infants. However, a study published in October 2014 indicates that elimination of tuberculosis by 2050 may require vaccines developed for adults and adolescents. The investigators used a mathematical model to estimate the impact and cost-effectiveness of a range of vaccination strategies in low- and middle-income countries. Gwen Knight, lead author of the study, said: “Dramatic levels of control are needed to eliminate tuberculosis and new vaccines need to be developed now. But because trials of vaccines are hugely expensive, their development needs very clear guidance. If elimination by 2050 is the goal, our study provides evidence that new vaccines should focus on targeting adolescents and adults rather than children.”

While finding an effective vaccine for tuberculosis is the ideal route for eradication of the bacterial disease, one must not lose sight of the forest for the trees. By all indications, an effective vaccine seems to be an elusive goal for the reasons indicated. While the search continues for a viable vaccine, the bacteria are becoming more antibiotic-resistant which is extremely detrimental to those infected. Possibly, in conjunction with the ongoing research on vaccine therapy, other mechanisms for the control of the disease should be considered.
Bonnie Bassler, a renowned molecular biologist at Princeton University, is an expert in the study of quorum sensing in bacteria. Quorum sensing is the ability of individual bacterial species to communicate with each other via chemical cell secretions called autoinducers. When the number of bacteria is sufficient, and the concentration of autoinducers is high, the bacteria can turn on their maximum virulence. The researchers at Bassler lab have developed ways in which to inhibit the quorum sensing capabilities of bacteria. This dismantling of intracellular communication results in an inability of the bacteria to attack in unison in an attempt to overwhelm the host’s immune defenses. Employing quorum-sensing therapy in conjunction with antibiotic therapy would provide individuals afflicted with resistant strains of TB a chance for their innate and adaptive immune responses to gear up and irradicate the infection. In doing so, they will develop a natural immunity to the infection while a vaccine is being developed.
Affecting the quorum sensing of the bacteria to supplement the vaccine is definitely a great idea. Actually, some of the vaccines that are being developed are supplements to the BCG vaccine. Although considering options other than vaccines to control the disease is wise, I think that there just isn’t enough focus on TB. TB has been known for a long time. But because of its prevalence in developing countries (and low income area) and lack of profitability, fighting against tuberculosis has been neglected. If we’re trying to eradicate TB by 2050, enough funding needs to be provided to increase the rate of progress in developing an effective vaccine.
Targeting the quorum sensing capability of Mycobacterium tuberculosis as a supplement to TB vaccination is a very interesting and conceivable approach; however, the success of this type of tactic would greatly depend on the extent of the bacteria’s utilization of quorum sensing during infection. A critical review published by researchers at the Indian Institute of Science discusses the quorum sensing (QS) mechanisms of mycobacteria species, including M. tuberculosis. The QS system regulates many bacterial behaviors, including the formation of biofilm. Since this mechanism is a direct result of QS, the scientists speculate that the biofilm forming molecules are most likely key actors in QS. Several species of mycobacteria have been shown to form biofilms in both in vitro and in vivo environments. M. tuberculosis has shown some characteristics of biofilm formation during in vitro infections. The TB-causing bacteria is also suspected of forming biofilm-like structures within in vivo granulomas; however, this conjecture has not yet been proven. In order to ascertain the effectiveness of QS inhibition techniques on M. tuberculosis, more research would need to be done to determine whether biofilm formation occurs during in vivo infections.
So, while the jury is still out on quorum sensing, let’s approach treatment of the Tuberculosis bacterium from a different angle, Mycobacterium Phage Therapy, otherwise known as Phage therapy. Mycobacterial phage is a virus that specifically target mycobacterium, such as Tuberculosis. These viruses work like viruses we are familiar with, in that they inject their DNA into the host cell, replicate, and then lyse the host cell releasing more mycobacterium phage to infect other bacterial cells. Research and development in phage therapy in the treatment of bacterial infections was in full swing, in both the US and Russia prior to World War II. Then antibiotics were discovered, and the US decided to put their R&D into creating a multitude of synthetic antibiotics. Russia, on the other hand, continued to develop phage therapy for bacterial diseases. Rusia has successfully treated localized skin ulcers, dysentery, Salmonella, Pseudomonas, and MRSA with phage therapy.1 Unlike synthetic antibiotics, bacteria do not seem to develop a resistance to phage, probably because of the evolutionary adaptability of the cellular receptors between the two species. Like the US, Russia does not have the TB epidemic that sub-Saharan Africa and Asia have. As a result, Russia’s research into phage treatment of TB has not been a priority. With all the successful treatments of bacterial infections with phage therapy, a combination of phage and antibiotics in the treatment of TB could be just around the corner.
1) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3278644/
Bacteriophage therapy against TB is a fantastic concept! From what I have read, in 1954 a mycobacteriophage was discovered that specifically targets virulent Mycobacterium tuberculosis. This phage has been found in soil samples as well as isolated from stool samples of tuberculosis patients. Recently, a drug-resistance reporter system utilizing these phages has been under development. This system would make it easier to test for antibiotic resistance in M. tuberculosis. These tests have shown high sensitivity in detecting resistance to the drug Rifampicin. In terms of TB treatment, more study definitely needs to be done. According to an article published in the Journal of Applied Microbiology, the mycobacteriophage DS-6A has shown high specificity for M. tuberculosis and seems to be a promising candidate for tuberculosis phage therapy. Early studies conducted on animals have been unsuccessful as the patients seemed to undergo toxic shock associated with the mass lysis of bacteria cells. An encouraging result from a 1981 study utilizing mycobacteriophage DS-6A exhibited lesion reduction in the organs of treated guinea pigs. Decreased granuloma formation resulted from this study, as well as others. A challenge of phage therapy against intracellular infections is that the phage must cross the macrophage cellular membrane and endure intracellular environments. This could be remedied by the development of phage delivery techniques. An additional challenge of TB phage therapy is that the mycobacteriophages may be unable to penetrate granulomas, thereby preventing total eradication of the bacteria from the body. In short, much more research needs to be carried out on this concept, which means more funding must be allotted for the effort. Unfortunately, due to patent complications, the incentive for research on phage therapy is minimal since pharmaceutical and other for-profit companies have less to gain from it than from drug development. Unless a massive TB outbreak occurs in a first world country, this research will probably be longwinded and mostly ignored.
An Oxford University lab in South Africa seems to be working on a BCG booster that would increase the efficacy against Mycobacterium tuberculosis. Their study uses “MVA85A…a recombinant strain of modified Vaccinia Ankara virus expressing the immunodominant M tuberculosis protein, antigen 85A”. Their aim was to boost infants in an endemic country where the cases of pulmonary tuberculosis at a young age is high despite the wide spread vaccination with BCG. The boost showed improved protection in animals, and showed “induced antigen-specific Th1 and Th17 cells, which are regarded as important in protection against tuberculosis”, in the infants studied. The Vaccinia virus has been used in other vaccinations (such as smallpox). These types of vaccines benefit from heat stability, low cost, and ease of administration. The trials have thus far shown higher and longer –lasting immunology to the Mycobacterium.
According the Nuffield Department of Medicine, The Oxford University Lab in South Africa did a trial involving the BCG booster, in that trial newborns were given the BCG vaccine at birth and half of them were given MVA85A booster between the ages of 4 to 6 months old. The results shown that the vaccine was harmless but it did stimulated weak immune responses and there was no improvement on the protection compared to BCG vaccine only. Now they are redirecting their focus on adolescents with them being the main reason for spread of the disease and reducing that will have a larger impact on the widespread disease. MVA85A is also better at generating an immune response in adolescents than in infants. They also feel that a stronger vaccine is needed especially in developing countries where tuberculosis is one of the major causes of death, so they are uniting with other vaccine developers to synthesize vaccines that will produce a stronger immune response. At the Oxford University Lab they are also looking at ways to immunize tuberculosis through the airways since that is the portal of entry.
Focusing on new ways to kill M. Tuberculosis, scientists at the John Innes center in the UK, collaborated with William Jacobs, an HHMI investigator, and discovered an enzyme essential for the bacteria’s survival. This enzyme is called GIgE; the bacterium uses it to convert maltose 1-phosphate to glucan which the bacterium uses for energy. Their experiments also showed that if they inhibit GIgE and maltose 1-phosphate accumulated in the bacterium then it would become toxic and substantially kill it. This is especially important because eukaryotic cells do not use this pathway and thus inhibiting the pathway would not negatively impact human cells. Drugs that inhibit this enzyme are in the process of being developed, even though it may not become available on the market for several more years, it may the a break that we needed. More resources should be devoted to these new methods.
Although focusing on adolescents and adults for a vaccine to TB is a good strategy for the elimination of TB, people with latent TB infections also play a role in the spread of the disease once symptoms begin. If given a vaccine to prevent the onset of disease, that saves the patient from undergoing TB treatment and those close to the patient from exposure. Researchers may have found a potential booster for children with latent TB infections and have already received the BCG vaccine. Scientists in a recent study (Early cellular immune response to a new candidate mycobacterial vaccine antigen in childhood tuberculosis) tested the use of the antibody heparin-binding haemagglutinin (HBHA) in children in order to test their initial immune responses to the antigen. They found that compared to non-infected children and children with active TB, that the most production of IFN-γ (cytokine that is secreted in response to active TB) was in children with latent TB infections and previously received the BCG vaccine. This gives BCG another reason to be used in the prevention of TB and gives children a quicker adaptive immune response to TB. Because of its limitations, there is still so far to go in the effort to eliminate TB, but it does bring us one step closer.
I agree with the contention that while focusing on the immunological mechanisms operating within older aged individuals infected with TB may provide a beneficial solution to the current TB epidemic, averting attention away from previously discovered aids of mitigation may not be wise. In particular, I feel that scientists may be closer than ever to identifying the prime components behind the immunological responses that hold the key to eradication of TB in both children and adults. For instance, as you stated earlier, the BCG vaccine has been found to produce a higher amount of cytokine IFN-γ in children with latent TB infections than those who were not infected or were suffering from active TB. Moreover in the same vein, a study by Kleinnijenhuis et al. titled, BCG-Induced Trained Immunity in NK Cells: Role for Non-Specific Protection to Infection ,revealed that injection of the BCG vaccine resulted in an increase of pro-inflammatory cytokines by NK cells in response to both mycobacterium and other unrelated pathogens in healthy individuals for up to three months following initial vaccination. Furthermore, although a change in the usual number and distribution of NK cell subsets not observed, it was also revealed that the induction of innate immunity within NK cells upon BCG vaccination and subsequent pro-inflammatory cytokine production further led to an accumulation of memory like NK cells with non-specific priming. Therefore, it can be inferred from this study that BCG vaccination has the potential for proving an immunologically protective basis, via innate immune cells, for not only mycobacterium but also unrelated pathogens, such as fungi. Consequently, findings such as these can not only broaden scientists’ prospects for TB eradication, but also the elimination/mitigation of other unrelated pathogens through an induced non-specific innate immune response.
There have been many cases in “middle-low income countries” that the BCG vaccine has been useful in preventing the spread of tuberculosis. The BCG vaccine was also used to prevent any communication with the HIV, human immunodeficiency virus, infection. The BCG vaccine is given to reduce the spread of bacilli from the site of infection. According to the article, the vaccination revealed 50% protection against mycobacterium tuberculosis in the lungs and “extra-pulmonary disease.” As tuberculosis is a latent infection, re-infection occurs rapidly which makes it very hard to predict the immune responses in individuals that have been exposed to tuberculosis and also those who have not been exposed. Although the BCG vaccine was not effective on tuberculosis, it was effective on individuals with HIV. According to the article, there was a study done in Africa on children who were HIV positive, and tuberculosis would not reactivate instead it would spread TB in the individuals as their immune systems are very weak; there was a higher chance of spreading tuberculosis in children with HIV. The cell-mediated response by T cells is a needed to “ control the spread of haematogenesis spread of the tubercle bacilli” because HIV causes the protection by the BCG vaccine to be ineffective.
I agree with your point. HIV causes the immune system of the host as it is an autoimmune disease. This virus is incredibly hard to fight because it is a retrovirus. As a retrovirus, its genetic material becomes part of the host cells it infects through reverse transcriptase. In addition, HIF infects CD4+ T cells macrophages, and dendritic cells. Logically it would seem almost impossible to teach our immune system to fight a disease which actively infects it. Countries most affected by TB are also highly affected by HIV and AIDS. These two diseases must not be thought of as separate; instead the fight against HIV and AIDS should also include the opportunistic pathogens which also when combined with a weak immune system causes death. As a person who took the BCG vaccine, I would love to see an advancement in the vaccine which may lower the risk in all individuals for TB. A good start is to reduce the risk of transmitting HIV in high-risk areas for the disease. Basic health education may prove to be effective, telling people to avoid bodily fluids, especially of those who have the virus seems like a logical first step.
The World Health Organization (WHO) observes March 24 to be World TD day. Tuberculosis (TB) is a bacterial disease of the lower respiratory system. The WHO states that, “young adults who are in their most productive age” is at risk for the TB infection. As often reiterated, TB is caused by bacteria (Mycobacterium tuberculosis) that infects the lungs. Moreover, the WHO states, “Tuberculosis is curable and preventable.”
With TB becoming increasingly drug-resistant due to the improper use of antibiotics and the and the likeliness of health care professionals to administer an antibiotic as the initial means of treating individuals in the health care setting is frightening. I am not trying to be a pessimist here; however, from a realistic standpoint what if an effective vaccine for TB is not developed by “2050” according to the “Stop TB strategy?” What will be the potential outcome of such deficits in offering an eradicative or potentially a life-saving remedy for TB-infected individuals?
As for the development of an effective vaccine that will eradicate the disease, the host/pathogen interaction within the immune requires a multiplicity of understanding. Author, Tortora gives insight into TB’s structural and biochemical characteristics. “Mycobacterium Tuberculosis is a slender rod and an obligate anaerobe.” The generation time for the rods is 20-hours or sometimes even longer.” Consideration should be taken in identifying why hosts’ resistance shows individual variations in responsiveness to the bacteria. An individual variation in responsiveness is an important point to note in the development of an effective vaccine will be given to mass populations for eradication purposes. One example is the incident which occurred in Lübeck Germany in 1929 where 249 babies were inoculated with a virulent strain of Mycobacterium instead of an attenuated vaccine. The inoculum was similar for all the babies; however, 76 babies succumbed and 173 did not become ill. Sufficient reasons offered by this incident warrants why extreme consideration should be placed at the level of the individual for TB’s vaccine development.
While reading the comments of my fellow colleagues, there seems to be intense research studies being carried out that will aid in the eradication of tuberculosis. Being a new parent of a 6-month old creates for me fear and concern for her well-being as it relates to her not being given the “Bacilli Calmette-Guérin” (BCG) vaccine. Since I now reside in the U.S., the vaccination guideline has vast differences. The Centers for Disease Control and Prevent (CDC) in 2015 issued recommendations for the vaccines that should be given to children from birth to age 6 and the BCG vaccine is not a part of that list. It is understandable why a concerned parent within the constraints of a new environ would find elusiveness in such a protocol. Information issued by TB Facts.org, states “the United States has never vaccinated all children,” because the level of TB in the U.S is not high based on WHO’s data.
According to WHO’s data, the incidence of TB in the U.S per 100,000 people is 0.0033. Moreover, its prevalence is 0.0041 as compared to Guyana’s incidence (the country where I receive my vaccine) 0.109, and TB’s prevalence is 0.129. As a child, I was given the BCG vaccine and as old as I am now, I can never be too certain that I will not succumb to an active TB infection. However, since I received the BCG vaccine, I have had no “fatal encounters,” or complications. Since I now reside the U.S. my daughter will not receive the BCG vaccine and as she becomes a young adult, should she encounter tuberculosis infection, how prepare will her immune system be to combat the disease? Just consider antibiotic resistance, multidrug-resistant (MDR) TB, extremely drug resistant (XDR) Tb, the undeveloped vaccine for eradication, 6-months treatment that can potential damage her liver is devastating to me.
The BCG vaccine administered to children offers some level of protection; however, the goal of the present research is the total eradication. One limitation of the BCG Vaccine is that it does not protect the broad spectrum of individuals inclusive of adolescents and adults holistically. The fact remains that there are always so many questions with no apparent answers to them. Therefore, the first step in the eradication of TB is learning how to prevent transmission. Again, it all comes down to individuals taking better stock of their health and exercising honesty about their health to health care workers within small knitted communities. If we all take on an “each one save one” ideology, then the first step to eradication can commence even without a vaccine.
It is exciting to live in a time in which we aim to eliminate tuberculosis as a public health problem but there will be several hurdles to overcome in order to reach our goal. First, we must manufacture an effective vaccine, but we also must be forward thinking in our approach and plan to not only manufacture a vaccine, but also deliver to the people in areas where tuberculosis is endemic. This could be just as daunting an obstacle as creating an effective vaccine itself due to the areas in which TB is endemic. Vaccines must maintain optimal conditions during storage and transportation; this is known as the cold-chain. If vaccines are not maintained at these optimal conditions the contents can denature and become ineffective. This can be particularly difficult in transportation of vaccines in underdeveloped nations in which refrigeration is not readily available. Unfortunately, many of the areas of the world in which TB is endemic tend to be underdeveloped areas. This means that even if we can manufacture an effective vaccine we need a way to maintain the cold-chain and deliver the vaccine to the areas most needed. Fortunately, there is work being done to create super insulating container to extend the cold chain. The goal of eliminating tuberculosis, as a public health problem is attainable but it will take contributions from both parties to manufacture an effective vaccine and delivery it efficiently to those in need in order to eliminate TB as a public health concern.
There are many campaigns which are contributing to promote healthy families, treating the diseases of poverty and mainly stopping Tuberculosis. According to the CDC, tuberculosis is the biggest killer of individuals in the world. Because it invades lymphatic system, TB can spread throughout the body. The use of resources and knowledge plays an important part in eliminating the spread of Tuberculosis. With having the right test, and performance and easy to use in all the levels of healthcare system can help diagnose Tuberculosis. Many individuals have latent TB. It is when the right diagnosis is made on individuals who have active TB and then treat them and protect their families and communities. Countries with high prevalence of TB will vaccinate children with BCG (bacilli Calmette-Guerin). To eliminate tuberculosis completely from USA and prevalent countries, new strategies is required. For example, CDC suggest the environmental control methods to eliminate TB. Also, According to the CDC article of Development of New Vaccines for Tuberculosis Recommendations of the Advisory Council for the Elimination of Tuberculosis (ACET) are researching and developing TB vaccines for clinically use on humans which includes DNA vaccines, attenuated strains of living bacteria and subunits vaccines) which could actually increase resistance and susceptibility to this bacteria. Individual’s immune system will be ready to fight off tuberculosis infection as quickly.
Making vaccines more accessible to third world countries where tuberculosis rates are much higher than anywhere else in the world is a good point. As indicated, since most vaccines can’t withstand certain temperatures and conditions and must be kept refrigerated until they reach their destinations, a good way to keep them viable is to have more efficient refrigeration, like the super insulating container that you mentioned above. However, in more recent years, researchers have started to develop dry forms of vaccines where refrigeration is unnecessary. One of these solutions is the Nanopatch. The Nanopatch is a small Nano chip-like silicon patch that contains about 20,000 projections coated with vaccine. These small projections enter through the outer layer of the skin, releasing the vaccine and targeting major skin immune cells. This pain free device has proven better efficacy than the standard syringe and needle. Because it is pain free, there is less of a chance for non-compliance to receiving vaccinations. It is also relatively cost effective. In countries where infectious diseases are already high and sanitation is not monitored, the Nanopatch assists in minimizing the spread of them. It does not require a needle, therefore cross contamination from reused needles and accidental needlestick injuries can be avoided. The patch is currently in it’s human trials, but it has been tests for several vaccines, including influenza, the human papillomavirus, and chikungunya. If the human trials are successful, a Nanopatch for tuberculosis would be incredibly convenient for those countries that are under developed and that do not have the proper resources to preserve vaccinations.