Cancer can spread from where it started (the primary site) to other areas of the body, forming metastasis. But how do cancer cells spread from the primary site to other areas of the body? When cancer cells break away from a tumor, they travel through either the bloodstream or the lymph system to reach other sites. If they travel through the lymph system, the cancer cells may end up in lymph nodes and grow inside them, forming lymph node metastasis. Usually, this process affects lymph nodes located near the primary cancer site — these lymph nodes are called draining lymph nodes, as they do most of the work to filter out or kill the cancer cells. At the same time, they are a staging area, and play a key role in advancing metastasis throughout the body when cancer cells are not killed. Between 29 and 37 percent of patients with breast, colorectal, and lung cancers are diagnosed with metastases in their tumor-draining lymph nodes.
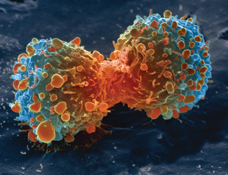
The super natural killer cells find the cancerous cells in the lymph nodes and induce apoptosis — in other words, the cancer cells self-destruct and disintegrate, thus averting their further lymphatic spread. But what are these super natural killer cells? They are a modified version of the so-called natural killer cells — or NK cells for short.
NK cells are a type of lymphocytes that play a major role in the killing of cancer cells and virus-infected cells by inducing apoptosis. To obtain the “super” version of these lymphocytes, scientists attached nanoparticles to the NK cell surface. These nanoparticles contain a protein dubbed TRAIL (Tumor necrosis factor Related Apoptosis-Inducing Ligand), which induces apoptosis by interacting with death receptors on cancer cells. But how does the system work in mice, exactly?
Mice are injected with nanoparticles containing TRAIL. However, in addition to TRAIL, the nanoparticles contain an antibody against a mouse natural killer cell marker. Once injected, the nanoparticles reach the draining lymph nodes, where they selectively attach to natural killer cell via the antibody. The TRAIL-armed natural killer cells, or super natural killer cells, then kill the cancer cells in a few days, and prevent lymphatic spread.
In January 2014, King and his colleagues published research showing that metastasizing cancer cells in the bloodstream could be annihilated by attaching the TRAIL protein, in combination with the E-selectin adhesion receptor, to natural killer cells. These cells were dubbed “unnatural killer cells.”
“So, now we have technology to eliminate bloodstream metastasis — our previous work — and also lymph node metastases,” King said in the press release.
Below is a video in which King explains his study on super natural killer cells that target metastasis in the lymph nodes.

Cancer is one of the hardest diseases to control and cure due to its variability and the unfortunate fact that symptoms of cancer usually don’t arise until a later stage, when it is more likely that the cancerous cells have metastases and migrated to the lymph nodes or other organs. I have a close family friend who only found out he had stage III colon cancer because he was in a horrendous motorcycle accident and upon treatment for his injuries they made the discovery. This leaves very little in the way of prevention for specific cancer types. Natural killer (NK) cells were originally thought to be categorized as an aspect of innate immunity. However, new evidence is suggesting that NK cells have memory capabilities and have blurred the lines between the two divisions of the immune system.
It seems promising that NK cells can be utilized to essentially stop cancer cells in their tracks. I am interested to see if there is any talk in place regarding using other lymphocytes such as B lymphocytes in this role as well. While there are new developments in further understanding the mechanism behind how cytotoxic T cells kill cancer cells, to my knowledge there aren’t any investigating the potential of B cell manipulation? B cells, upon activation, transform into plasma cells and pump out swarms of antibodies for months in order to defeat a pathogen and preserve the viability of the host. It would be interesting to see if there was a way to manipulate the B cell antibody production (perhaps with TRAIL or a similar nanoparticle) which can stimulate the antibodies to neutralize cancerous cells and enhance the ability for the immune system to stop the cancer metastasis.
This research shows the variability in the types of cancer metastasis that can be halted in the lymph nodes and eliminated before it involves other organs. Perhaps unlocking the ability to utilize other lymphocytes may further enhance the tumor defeating abilities by being able to prevent metastasis in other parts of the body in addition to the lymph nodes.
After reading your post, particularly where you asked if B cells manipulation has been done, I decided to do a bit of research on the subject. The general feeling that I’ve gotten from looking at a few research and review articles is that we currently do not know as much about B Cells’ role in fighting cancer than T or NK cells. One of the big players in B-Cell regulation of cancer, namely Breg (aka regulatory B Cells) were only recently discovered, so not much is known about them. Some research is showing that they help suppress the expression of inflammation cytokines, but it also appears that they may actually be facilitating cancer growth through their suppression of cytokines. It also appears that Bregs may act as an immunosuppressant by inferring with the production of CD4, CD8, and plasma cells. I haven’t seen any research beyond this, but it sounds like understanding the full mechanics behind Bregs may be a key to pushing the cause for curing cancer along.
Here’s the link to the article I found:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4060293/
I was always curious about how cancer “spread” from one area of the body. It never made sense to me how cancer from in one part of the body leads to cancer in another, often unrelated, part of the body. It makes sense that a tumor cell could break off and travel elsewhere, and I am very happy to see that this research is a huge step forward in preventing metastasis. However, one question I do wish was addressed in the article, and perhaps even the primary researchers do not know the answer either, is why does the TRAIL protein only work on a tumor cells that are metastatic? It seems logical to assume that a protein like TRAIL would be able to attach to the cells that make up the original tumor as well. Perhaps future research could look into the possibility of coating the tumor itself with TRAIL to induce massive apoptosis of the primary tumor.
Combating cancer is a rigorous process, and without a doubt, body’s own immune system plays an important role in such process. Nature Killer (NK) cells are part of the innate immune cells that responsible for inducing apoptosis to tumors and pathogen infected cells using toxic granules that carried with it.
As the blog stated, King and his colleagues develop a protein call TRAIL to boost its effectiveness against metastasis cancer cells in the lymph nodes. It is fascinating and interesting for me to see a study in boosting NK cells to combat against cancer. But my questions is that how do the new “super NK” cells recognize and distinguish the cancer cells rather than the healthy cells. Another the big problem for NK cells therapy is that the rapid loss of activity, hence it aggressiveness, but as for cancer cells they’re constantly dividing and mutating. Aside from these two problem, NK cells also made up of only 10% of all the lymphocytes in the body therefore this research could be a precursor for future development of TRAIL homolog that could attach and increase the function of T-cells in combating cancer.