Dendritic cells and T lymphocytes play together to ensure immunological tolerance—a functional state in which T lymphocytes are unable to respond to certain antigens. Why is immunological tolerance necessary? The answer is simple: T lymphocytes must be able to direct their destructive potential to infected cells and cancer cells while, at the same time, avoiding to attack healthy cells. In other words, T lymphocytes must be able to respond to foreign antigens while tolerating self-antigens. Such self/non-self discrimination is essential to avoid autoimmune responses. Understanding the mechanisms that lead to immunological tolerance is crucial to advance the development of therapeutic strategies for the treatment of autoimmune diseases, and to improve the outcome of organ transplantation.
According to Daniel Hawiger, dendritic cells “are the music directors, telling other lymphocytes such as T cells what to do and how to do it.” Hawiger is the senior author of a study recently published in the journal Immunity. The study (Immunomodulatory Functions of BTLA and HVEM Govern Induction of Extrathymic Regulatory T Cells and Tolerance by Dendritic Cells) helps to understand how dendritic cells direct T lymphocytes to learn tolerance for the body’s own antigens. “T cells are the immune system’s fighters,” Hawiger said. “Dendritic cells help train T cells to distinguish between self and non-self.”
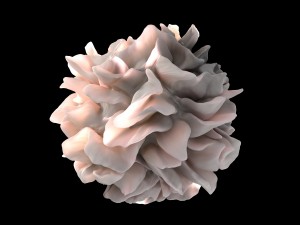
Dendritic cells were first described by Ralph Steinman in the 1970’s and, since the 1980’s, it has been known that one of the major functions of dendritic cells is antigen presentation—the display of peptides derived from viral and cancer antigens to T lymphocytes. Following recognition of peptides, T lymphocytes become activated and initiate a complex set of events. These events require the participation of different immune cell types and may lead to the elimination not only of cells infected with viruses, but also cancer cells. However, results obtained in the past few years indicated that, in absence of pro-inflammatory stimuli, activation of T lymphocytes by dendritic cells results in tolerance—T lymphocytes will not become activated following presentation of peptides. Induction of tolerance is mediated by a particular type of T lymphocytes—the so-called T regulatory cells.
Now, results from the new study by Hawiger’s team show that, in contrast to what previously believed, the presentation of antigens to T lymphocytes by all dendritic cells in absence of infection and inflammation does not lead to the induction of tolerance, and it does not lead to immunity. Rather, it causes short term activation of T cells, but no long term effects. In addition, results from the new study show that tolerance can be induced only when antigens are acquired and then presented to T lymphocytes by a specialized group of dendritic cells. These specialized dendritic cells carry on their surface a protein called B and T lymphocyte attenuator, or BTLA for short. BTLA gives specific signals to T lymphocytes by interacting with a receptor—called herpes virus entry mediator or HVEM—located on the surface of the T lymphocytes. Induction of tolerance occurs only in presence of these specific signals.
Hawiger said: “I hope this new information may help us more precisely regulate the immune response. In the case of an illness like multiple sclerosis, where the immune response is causing damage, we may be able to develop a therapy that will dampen that response. Perhaps we can harness these functions and learn to turn the volume up or down, in response to the needs of those with a variety of health concerns, and in particular, autoimmune diseases.”

This study does a great job at giving us a small window into how the immune system functions. Understanding the mechanisms that fuel attacks on healthy cells by our own immune systems is vital. Research like this is how we will make strides in treatments and cures to better the immune system. The T cells controlled by these specialized dendritic cells are key players when it comes to autoimmune disorders and if we can control how these B and T lymphocytes are regulated we can get the upper hand on fatal autoimmune disorders. This finding is also significant when it comes to transplant research. We are getting closer than ever to transplantation resulting in 100% acceptance by the host’s body. Granted the research is far off but this is a step in the right direction.
With the understanding this study gives us of the role of B and T lymphocyte attenuator (BTLA) we can consider looking into the other roles of this protein and our bodies cells. A study done in October of last year touches on another important role of the protein. The study Clinical significance of tumor-infiltrating immune cells focusing on BTLA and Cbl-b in patients with gallbladder cancer looks into the role of BTLA in cancer cells, specifically gallbladder cancer. What the researchers found was that BTLA along with other vital cell receptors can function as an indicator for patient survival. They also found that BTLA plays an important role in inhibiting antitumor immunity. With enough understanding of this protein and its receptors we have the possibility of controlling it. Being in control means control of tumor mechanisms and enhanced tumor immunity. This research does not just effect autoimmune disorders but a wide range of ailments.
https://www.ncbi.nlm.nih.gov/pubmed/26395180
Utilizing the knowledge regarding the necessity of the interaction between BTLA and HVEM it can be reasonable to want to try to carry out studies to induce their interaction to enhance exposure therapies utilized to treat people suffering from allergic reactions. First studies would have to be oriented to try to determine pathways that can be utilized to induce the interaction between BTLA and HVEM while cataloging how the other facets of the immune system may be affected by their enhanced activity. If it would be found to be possible to utilize BTLA induction along with exposure therapies it could shorten the time necessary for the person to build up tolerance to the allergen while likely further enhancing the likeliness that such tolerance does not wane with time.
It would be necessary to get a firm understanding on the activities of both BTLA and HVEM for any plans regarding utilizing them as one of the foreseeable consequences could be leading to the immune system developing tolerance to a pathogenic peptide rather than activating a T-cell. Any method employed would have to possess high specificity or use along with dosage of immunoglobulins to protect the body from possible opportunistic pathogens while the immune system would be building tolerance based on BTLA induction.
It’s kind of humbling to think about “modern medicine” and the fact that dendritic cells were only just discovered in the 70s, and their major function in the 80s, just 3 decades ago. Yet at the same time, the amount of information we’re gaining every decade makes it an exciting time to be alive. Because of this rapid increase in technology, I imagine we’ll one day look back on our recent approaches to medicine in the same way we currently look back and laugh at leaches being used to balance the humours. Indeed, many of the current approaches to dealing with autoimmune diseases involves the application of non-specific agents to suppress effector cells in mass. This kind of blindfolded approach to autoimmune treatment often comes with serious, if not life threatening, side effects. Fortunately, as our understanding of immunity has increased, particularly with regard to dendritic cells, their function, and their relationships with T cells, so too has our finesse and specificity in potential treatments to autoimmune disorders.
Tolerogenic dendritic cells (tolDCs) are dendritic cells that help weed out self-targeting T cells and help the body maintain self-tolerance. Consequently, they’ve been a huge focus for many new therapeutics in the laboratory. Some of the therapeutics I’m particularly interested in feature engineering human tolDCs ex vivo with the ability to properly respond to an existing autoimmune disorder and then integrating these engineered dendritic cells into the patient. Again, it’s amazing to consider where the science of the field has come in such a short time span, and where it’s headed.
Citation: Brussel IV, Lee WP, Rombouts M, et al. Tolerogenic dendritic cell vaccines to treat autoimmune diseases: Can the unattainable dream turn into reality? Autoimmunity Reviews. 2014;13(2):138-150. doi:10.1016/j.autrev.2013.09.008.
Specialized dendritic cells communicate with T lymphocytes on immunological tolerance. Dendritic cells http://lab.rockefeller.edu/steinman/dendritic_intro/immuneTolerance
are always monitoring the tissues and engulfing antigens from dead cells. They process and present harmless and nonpathogenic antigens to the T lymphocytes more often than not. To avoid wasting energy and resources, these dendritic cells process and present the antigen to a unique T lymphocyte that will recognize it but will not become activated. However, activated in this sense means the T cell will not produce the effector cells that are the backbone of immunity; but instead produce regulatory T cells. The regulatory T cells will suppress the reactions of other immune cells, thereby avoiding autoimmune disease.
The blog post describes that it is the lack of infection and inflammation that triggers immunological tolerance. Infection and inflammation are signs of an invader that can harm a systemic process or organ. Thus, under those conditions dendritic cells are charged with a different task. Dendritic cells are the connection between the innate immune response and the adaptive immune response. They mediate the processes that directly eliminate a pathogen.
I can see how understanding this phenomenon affects organ transplant recipients. Surgeons have to evaluate whether a patient is a good candidate for a transplant. Nonetheless, recipients can still reject the transplant. This happens if the body sees the organ or tissue as a foreign invader and attempts to destroy it. There are two types of rejection, acute and chronic. http://organdonor.gov/about/process/transplant-process.html
Acute rejection occurs immediately with signs of infection and inflammation of the organ. Chronic rejection is the prolonged failure of the organ to function. Immunosuppressant medications are a critical part of the recipient’s life after transplantation. Immunosuppressant drugs block the immune system from defending the body from foreigners and subsequently reduces the chance of rejection. Unfortunately, these drugs make the organ recipient susceptible to other infections and slower to recover from illness.
Porsha, I like that you focused on organ transplant rejection and wanted to look into the role of BTLA and other proteins that may be involved in rejection by the host. I was able to find a recent article on T-cell mediated rejection (TCMR) in kidneys and what causes this rejection. What they found was that it was a “hierarchy of T cell signaling”. They also found not only that TCMR was associated with BTLA but other transcripts like CTLA4, and IFNG. They were able to use different studies to try to track the varying proteins involved in rejection and one good thing that came out of their study is that they found evidence that the players are consistent. They found that effector T cells and NK cells play the biggest role in this kind of rejection. Knowing this and some of the signal details will hopefully give us better insight into how our own immune system can attack our own cells. Once we understand why it’s happening hopefully we can stop it. This would be a breakthrough in the transplantation research field.
Citation: Venner, J. M., Famulski, K. S., Badr, D., Hidalgo, L. G., Chang, J. and Halloran, P. F. (2014), Molecular Landscape of T Cell–Mediated Rejection in Human Kidney Transplants: Prominence of CTLA4 and PD Ligands. American Journal of Transplantation, 14: 2565–2576. doi:10.1111/ajt.12946
Autoimmunity is major life threatening condition and as complicated as infection and cancer. The switch between immune tolerance and immune response has not been identified clearly before this current study. It is an amazing study to understand how the both the system distinguish between both the mechanism by a simple phenomenon of attaching a marker on the dendritic cell and indicate the Tcells how to function further.The different receptors like BTLA, LIGHT, HVEM has to be studied further. BTLA becomes highly expressed on T helper 1 (TH1)-polarized cells, but is absent from TH2-polarized cells (indicated by a star). Immature DCs express high levels of both HVEM and LIGHT, and lower levels of BTLA. With maturation, the expression of both HVEM and LIGHT decreases in DCs, but, contrastingly, the expression of BTLA in bone-marrow-derived DCs increases with maturation.to correlation among these markers are not fully understood. However I feel it is a small gateway which opened for multiple possibility in treatment against immunomimetic conditions, autoimmune diseases, and various cancer treatment.The pathway make the BTLA activation is yet to be known. The major role of dendritic cells in immune response has been revealed by the current study however further markers and its role has to be identified yet to establish sound understanding recent study conducted in mouse showed Lack of B and T lymphocyte attenuator exacerbates autoimmune disorders and induces Fas-independent liver injury. The multiple role of each markers has to be established for the better understanding possibility investigation in treatment.
Citation:
Balancing co-stimulation and inhibition with BTLA and HVEM Kenneth M. Murphy, Christopher A. Nelson & John R. S caronedý
Nature Reviews Immunology 6, 671-681 (September 2006) doi:10.1038/nri1917
Lack of B and T lymphocyte attenuator exacerbates autoimmune disorders and induces Fas-independent liver injury in MRL-lpr/lpr miceInternational Immunology, Vol. 23, No. 5, pp. 335–344
It would be interesting to see the mechanism by which these two receptors mediate immunity. My lab has discussed the HVEM receptor at lab meetings a few times and to my knowledge we have never discussed the mechanism behind dendritic cells BTLA and HVEM mediating the induction of tolerance via these two receptors.
We have come to learn the immense role of antigen processing and presentation plays in mediating our adaptive immune response. The delinquent interplay between dendric cells and T lymphocytes, as mentioned in Hawiger’s paper, is a symphony in motion. And yet the vastness of our ignorance is awe-inspiring. Needless to say, we have much work before us. While reading this blog post and associated source material and learning about the role of these specialized dendritic cells I was struck by the irony of a specialized subset of an already specialized group of cells. From my understanding, meager as it may be, dendritic cells are already specialized and derive from a hematopoietic lineage which is distinct from other members of the leukocyte family (1). The question that immediately came to mind was why? Why have a unique subset such as these BTLA dendritic cells? My first thought was, of course, evolution. There must have been some adaptive advantage to some long lost ancestor of ours. Unfortunately, I was unable to find relative research to answer my question, merely molecular characterization of the binding site between BTLA and HVEM. It appears that my question will remain unanswered, for now.
Citation:
1. Merad M, Sathe P, Helft J, Miller J, Mortha A. The dendritic cell lineage: ontogeny and function of dendritic cells and their subsets in the steady state and the inflamed setting. Annu Rev Immunol. 2013;31:563-604. doi: 10.1146/annurev-immunol-020711-074950.
This is how science advances, by challenging what we thing to be be true and proving otherwise using the advances in technology. For some reason I am unable to access the article and read through it and because of this it is difficult for me to assess how well the work was done. But Arya has cited a paper titled “Balancing co-stimulation and inhibition with BTLA and HVEM” by Kenneth M. Murphy which proposes that there is some merit to what was documented in this paper. If what the author Daniel Hawiger published is true that was a great find.
The study mentioned in this post appears to be a great starting point for potential therapies for autoimmune disorders with T regulatory cells as targets. The factor FoxP3 plays an integral role in the functioning of T regulatory cells. A loss in function of FoxP3 results in an increase in circulating antibodies and throws immunological homeostasis out of wack. Depletion of T regulatory cells can be the cause of autoimmune reactions and dysfunction. (Wing, James B., and Shimon Sakaguchi. “Foxp3+ Treg cells in humoral immunity.” International immunology (2013): dxt060.) Perhaps the gene locus controlling FoxP3 could be used in up or down regulation of T regulatory cell function, thereby providing a therapeutic effect in those with autoimmune disorders.
It is overwhelmingly astonishing that the cells in our body have the ability to distinguish between self-antigens and antigens of foreign substances. This ability is crucial in regulating autoimmune disorders that lose the ability to make this distinction. I was intrigued to find out about the correlation between Multiple Sclerosis and antigen-specific tolerance. Ideal therapy for inflammatory diseases within the nervous system would preserve normal immune function and suppress the pathologic immune response that damages tissues and allows for repair. I pondered what antigens drive inflammatory responses in MS pathology. In recent studies it has been shown that there is no known particular antigen in which drives the inflammatory response in MS. There are, however, T-cell and humoral responses that have been detected for all of the known myelin proteins. (1) Also, in a recent study it has been shown that there is a failure of activation of induced cell-death (AICD) in T lymphocytes from pts with MS which demonstrated that PHA-induced AICD was reduced in T lymphocytes from pts with relapsing-remitting MS compared with controls. (2)
References
(1) Steinman L. The re-emergence of antigen-specific tolerance as a potential therapy for MS. Multiple Sclerosis Journal [serial online]. September 2015;21(10):1223-1238. Available from: Academic Search Complete, Ipswich, MA. Accessed November 13, 2016.
(2) Moreno M, Negrotto L, Comabella M, et al. Activation-induced cell death in T lymphocytes from multiple sclerosis patients. Journal Of Neuroimmunology [serial online]. July 15, 2014;272:51-55. Available from: ScienceDirect, Ipswich, MA. Accessed November 13, 2016.
Sonya,
The articles you cited were eye opening in beginning to understand the complexity of the immune system and specifically when its activity goes awry. I too am interested in the underlying mechanisms contributing to MS. A study out of Germany showed the connection with IL-1, but their findings are preliminary at best (1).
Citations:
1. Mufazalov IA, Schelmbauer C, Regen T, Kuschmann J, Wanke F, Gabriel LA, Hauptmann J, Müller W, Pinteaux E, Kurschus FC, Waisman A. IL-1 signaling is critical for expansion but not generation of autoreactive GM-CSF+ Th17 cells. EMBO J. 2016 Nov 8. pii: e201694615.
This information successfully enlightens me about even more reasons why dendritic cells prove to be pivotal in the immune system’s overall function. The dendritic cells usually orchestrate the activation of T cells and modulate the T cells’ ability to recognize self and non-self-molecules. This simple self-recognition may make or break one’s ability to avoid autoimmune disease. The function of T regulatory cells may have suppressive functions on these T cells that do malfunction. Dendritic cell function and T cell self/non-self-recognition is a function dependent upon two factors: the presence of a specialized group of dendritic cells and the presence of cell surface protein BTLA. These accumulation of knowledge such as the facts learned in these studies continue to move society closer toward medical advances including immunotherapy for the treatment of cancer.
Immunological tolerance is necessary so that T lymphocytes only destroy the infected and cancer cells and at the same time doesn’t cause any harm to the body’s healthy cells. This blog post cites a study where the researchers show that induction of tolerance requires the interaction of BTLA which is a protein present on the surface of dendritic cells and HVEM- a receptor located on the surface of T lymphocytes. While I was trying to figure out what are the other roles of BTLA and HVEM in general in our body, I came across very interesting study. In this study(1), the researchers revealed a new role for the BTLA-HVEM pathway in promoting the survival of activated CD8+ T cell in the response to an oral infection with intracellular bacteria Listeria monocytogenes. In this study, both BTLA- and HVEM-deficient mice infected with Listeria monocytogenes had significantly reduced numbers of primary effector and memory CD8+ T cells, despite normal proliferation and expansion compared to controls. In addition, blockade of the BTLA-HVEM interaction early in the response led to significantly reduced numbers of antigen-specific CD8+ T cells. HVEM expression on the CD8+T cells as well as BTLA expression on a cell type other than CD8+ T lymphocytes, was required.
This study clearly demonstrated that the function of the BTLA-HVEM pathway is not limited to inhibitory signaling in the responding T lymphocytes, and instead, that BTLA can provide crucial, HVEM-dependent signals that promote survival of antigen activated CD8+ T cell during bacterial infection.
Citation:
1. Steinberg MW, Huang Y, Wang-Zhu Y, Ware CF, Cheroutre H, Kronenberg M. BTLA Interaction with HVEM Expressed on CD8+ T Cells Promotes Survival and Memory Generation in Response to a Bacterial Infection. PLoS ONE 2013, 8(10): e77992.
The NIH estimates that nearly 23.5 million people in America suffers from autoimmune (1) disease and is steadily rising. There are 80-100 different autoimmune diseases and there are about 40 additional diseases that are relate to autoimmunity. These diseases are chronic and can be life threatening. Currently there is no known cause. The article explains that dendritic cells that did not express BTLA are not able to induce T regulatory cells. The presence of BTLA on dendritic cells is able to engage HVEM which then promotes Foxp3 expression in T cell through upregulation of CD5. It goes on to say that T cells activated in the absence of BTLA and HVEM-mediated functions remained CD5 low and failed to resist the inhibition of Foxp3 expression. The interaction of BTLA and HVEM are key players in T regulatory activation.
BTLA may possibly allow researchers to understand cause of autoimmune disease. In one study (2) it explains that the lack of B and T lymphocytes attenuator exacerbates autoimmune disorders.BTLA can possibly be the first key to understanding the mystery of autoimmune diseases.
(1) http://intimm.oxfordjournals.org/content/23/5/335.full.pdf
(2) https://www.aarda.org/autoimmune-information/autoimmune-statistics/